Tackling the Complexity of Healthcare EOB Processing
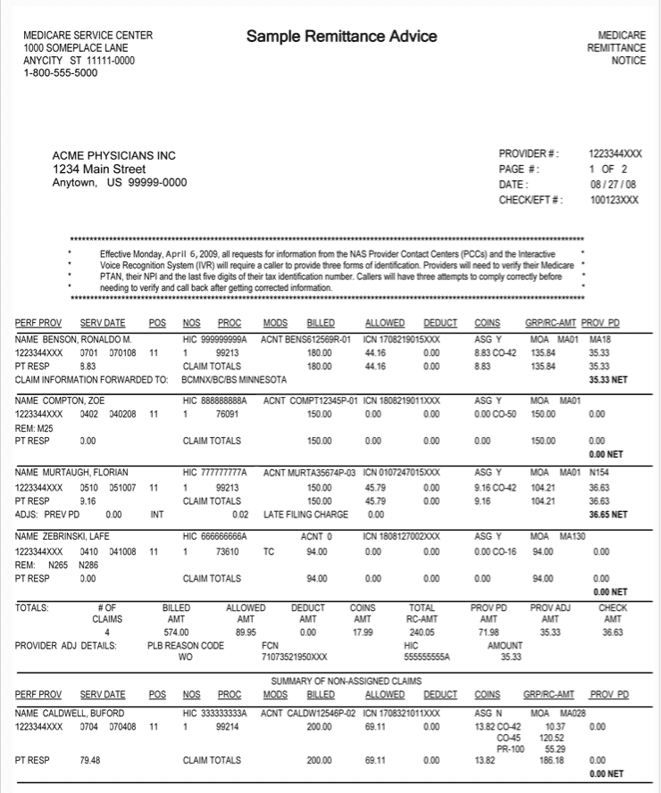
In the intricate world of healthcare administration, processing Explanation of Benefits (EOB) documents represents one of the most challenging document extraction tasks. These complex, multi-page statements—containing detailed payment information across numerous claims—have traditionally required extensive manual processing, creating bottlenecks in healthcare revenue cycle management.
Eagle Doc has developed a specialized AI-powered solution that transforms this labor-intensive process into an automated, efficient workflow with exceptional accuracy.
The EOB Processing Challenge
Explanation of Benefits documents present numerous extraction challenges that defeat conventional OCR solutions:
- Complex Multi-Page Tables: EOBs contain intricate tables that span multiple pages with varying formats and structures
- Dense Information: Each document includes detailed claim information, payment adjustments, provider details, and patient information
- Inconsistent Formatting: Different insurance providers use different formats, layouts, and terminology
- Code-Heavy Content: EOBs contain numerous specialized codes (procedure codes, adjustment codes, etc.) that must be accurately captured
- Variable Quality: Many EOBs arrive as scanned documents with varying levels of image quality
- Maintaining Context: Information in EOBs requires contextual understanding across different sections and pages
Eagle Doc's Specialized EOB Processing Solution
Our AI-powered document understanding system has been specifically trained to handle the complexities of healthcare EOB documents:
- Advanced Table Recognition: Our technology precisely identifies and extracts multi-page tables with their hierarchical structure intact
- Intelligent Field Extraction: The system accurately captures critical data points including:
- Patient information and member IDs
- Provider details
- Claim numbers and dates of service
- Procedure codes and descriptions
- Billed amounts, allowed amounts, and payment amounts
- Adjustment codes and reasons
- Patient responsibility calculations
- Contextual Understanding: Our AI maintains relationships between interconnected data elements across the document
- Format Adaptation: The system works across various EOB formats from different insurance carriers
- Quality Enhancement: Built-in image preprocessing optimizes document quality before extraction
Business Benefits
Healthcare organizations implementing Eagle Doc's EOB processing solution experience transformative results:
- 95%+ Extraction Accuracy: Significantly higher than traditional OCR systems on complex EOB documents
- 80% Reduction in Processing Time: What once took hours of manual work is completed in minutes
- Accelerated Revenue Cycle: Faster processing leads to quicker payment posting and improved cash flow
- Reduced Labor Costs: Staff can be redirected from manual data entry to higher-value tasks
- Improved Compliance: Consistent processing reduces human error and helps maintain regulatory compliance
- Enhanced Analytics: Structured, digitized EOB data enables better analysis of claim patterns and payer behaviors
Seamless Integration
Our EOB processing solution is designed to fit seamlessly into existing healthcare workflows:
- API-First Design: Simple integration with practice management systems, billing software, and revenue cycle management platforms
- Flexible Deployment: Available as cloud-based service or on-premises installation
- Batch Processing: Handles high volumes of EOBs efficiently
- Structured Data Output: Delivers extracted information in standard formats (JSON, CSV, XML) ready for import
The system can be customized to extract additional fields specific to your organization's needs and integrated with your existing document management systems.
Case Study: Multi-Specialty Medical Group
A large multi-specialty medical group with over 200 providers was processing approximately 5,000 EOB pages monthly, requiring 4 full-time staff members dedicated solely to manual data entry. After implementing Eagle Doc's EOB processing solution:
- Processing time decreased by 85%
- Staff was reduced to 1 verification specialist
- Payment posting lag was reduced from 7 days to same-day
- EOB-related data entry errors decreased by 96%
- Annual cost savings exceeded $180,000
The practice was able to reallocate staff to patient care support and insurance follow-up tasks, improving both revenue cycle performance and patient satisfaction.
Transform Your Healthcare Revenue Cycle with Eagle Doc
Stop letting manual EOB processing create bottlenecks in your revenue cycle. Eagle Doc's specialized AI solution delivers unprecedented accuracy and efficiency in processing even the most complex healthcare EOB documents.
Frequently Asked Questions
How does Eagle Doc's solution handle different EOB formats from various insurance providers?
We use advanced AI models that can adapt to a wide variety of EOB formats without needing custom training for each provider. This allows us to deliver high accuracy right out of the box.
What level of accuracy can we expect compared to manual processing?
Our EOB processing solution consistently achieves over 95% accuracy in field extraction—significantly outperforming manual data entry, which typically ranges between 80–85%.
How quickly can we implement the Eagle Doc EOB processing solution?
Most customers are up and running within 1–3 days. We provide seamless integration with your existing systems and tailor the solution to your specific EOB formats. Our team collaborates closely with your IT and revenue cycle teams to ensure a smooth, disruption-free rollout.
Is the solution compliant with healthcare privacy regulations?
Yes, our solution is fully designed with compliance in mind. We never store documents on our servers—files are processed in real time and deleted immediately afterward to ensure data privacy and security.